At first, Amandip Sidhu was puzzled by the email from his brother, Jagdip, that flashed up in his inbox in the middle of the afternoon. It was a confusing list of instructions, including how to access his financial accounts, life insurance policies, when to get the car MOT’d. There was no explanation. It ended with a short sign-off — he had gone to Beachy Head, a beauty spot atop the cliffs of the South Coast, with the car.
Maybe his brother had decided to spend some time in the countryside, Amandip thought. But as call after call went straight to voicemail, the panic started to set in. He called Jagdip’s wife — there was no sign of him at home. He had left without taking his wallet and house keys. Amandip raced across London to his brother’s house. When he arrived, it was already crawling with police. They had found the car by Beachy Head, but there was no sign of Jagdip. Coast Guards and sniffer dogs had been deployed. And Amandip waited.
An agonising two hours later, he heard the crackle of the officers’ radio as they walked into the room and started to speak. “I remember them saying 'This is the part of the job I really hate',” Amandip recalls. They had found his brother’s body, identified by the car keys that were still in his pocket. Jagdip was 47 years old.
There were a lot of questions in the blur of weeks and months afterwards. But above all, one thought increasingly haunted Amandip: did his brother's job in the NHS play a role in his death?
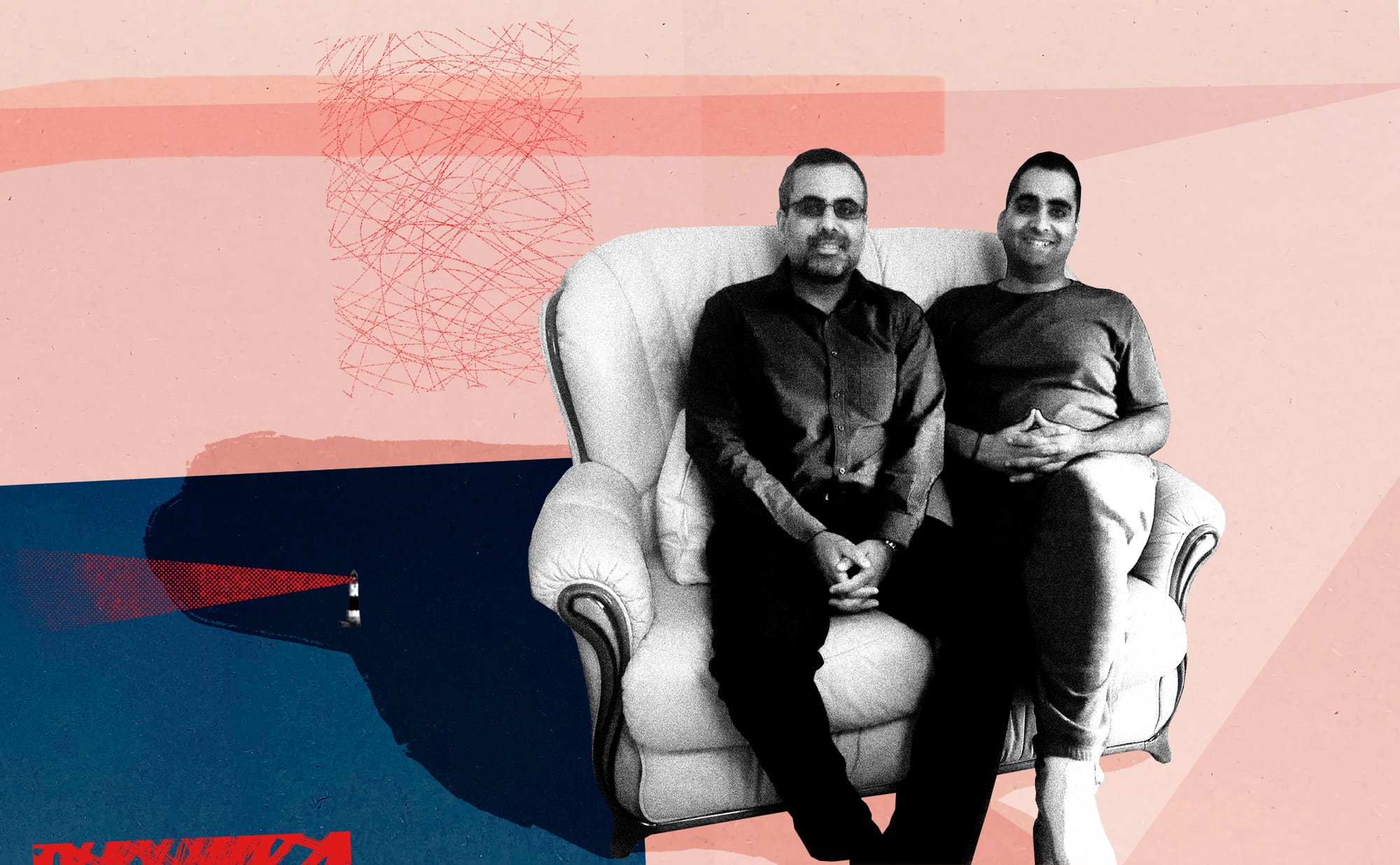
We’re sitting in the dining room of Amandip’s home in Watford, just a few miles from where the brothers grew up in Hatch End. With greying cropped hair and a slightly weary expression, he gently taps a small green stress ball against the table while we speak. Occasionally, as he delves deeper into his brother’s life, the tapping becomes more frantic.
The siblings were born in East Africa, but their parents moved to northwest London in 1977, when Jagdip was six and Amandip was one. Their early life in Hatch End was almost stereotypical, by Amandip’s account — a suburban life of leafy streets and good schools — despite being “the only non-white faces” in the area. A perfectionist and a people pleaser with a “maturity beyond his years”, his brother reacted to their position as new arrivals by working harder than everyone else in school; to prove “we can fit in, we can assimilate”, as Amandip explains it.
The family idolised him. To their dad, he was the perfect son; the straight-A student he could boast about. To Amandip, he was the protector. They weren’t at all alike — Amandip pushed against his parents’ expectations much more — but Jagdip was the older brother who brought him to hang out with his friends, and who defended him when his dad vented his frustrations at Amandip for failing to match his standards. His teachers loved him too, glad of such a perfect pupil. When Jagdip started studying for A-levels, he decided he wanted to do an extra subject — physics. The school said they didn’t have the capacity to teach him. But he did it anyway, teaching himself using textbooks borrowed from libraries. He got straight As. “He always wanted to be a doctor,” explains Amandip. Not for the renown and certainly not for materialistic reasons — he spent much of his life driving a Skoda — but for the challenge, validation and, hopefully, independence; “the ability to live life as he chose,” as Amandip puts it.
After finishing medical school, Jagdip worked at Ealing Hospital. He was thrown in at the deep end. The hospital was “complete chaos”, says Amandip, a never-ending conveyor belt of patients and procedures and not enough people to do them. But he threw himself into the job and would return home exhausted, shoes tattered and feet covered in blisters from a day spent walking ten miles back and forth across the hospital, and fall asleep on the family sofa. After his training, he decided to specialise in cardiology. It wasn't as highly paid as neuroscience or surgery, but it was a field where he could make a difference. Plus, it wasn’t as filled with gore as frontline surgery. He moved across various hospitals in the capital as he finished his specialism training, and got married and had two children. Eventually, he took a job running the cardiology department at Darent Valley Hospital in Dartford, and moved to the southeastern border of the capital with his family.
Jagdip was the platonic ideal of an NHS doctor. He took very little private work, despite it being common for consultants. His only exception was for those who needed urgent care that couldn’t get treated on the NHS. It was a point of ethics. “He said: I'm only going to do it for people who clinically cannot wait,” explains Amandip. “I'm not going to sit and profit off people's adverse health and misery.”

In 2007, their dad died of heart failure, the same problem Jagdip spent his working days treating. “He tried everything to save him, every treatment,” his brother recalls. “It just wasn’t enough.” Over the ensuing decade, the constant demands of his job started to weigh him down more and more. To try and cope, he had his escapes. He was a keen swimmer and enjoyed hiking through nature. He often came back to Harrow to visit his family and go out to dinner at the area’s good Indian restaurants. And he loved to travel, nowhere more than Switzerland. Surrounded by towering mountains, he would find a sense of serenity away from it all.
But the hospital was impossible to get away from. On days and nights off, he would get urgent messages from the managers at his NHS trust asking him to clear more beds on the ward or hit new performance targets. Gradually, he had less time for anything outside of work. More and more of his whole identity was being subsumed by his job. There was room for little else. He’d developed “tunnel vision”, as Amandip describes it.
By 2017, something had broken in him. “He had just suddenly aged,” recalls his brother, pausing for a moment before continuing. “It's very hard to explain. But for someone who had a lot of vitality in life and charisma about him, it started to drain away.” His hair began to turn grey. He was constantly tired, surviving on just three or four hours of sleep each night and often working more than 14 hours a day. “He'd come and see mum and literally just pass out on the sofa,” recalls Amandip. He spoke less and less. Jagdip was also losing faith in the medical system whose values he once embodied, and confided to his brother that he thought the struggling NHS was “finished”.
In November 2018, things hit breaking point. One Thursday, Amandip got a call from his brother. “I saw his number flash up, and I knew something was wrong,” he recalls. Jagdip explained that he had been signed off work on medical leave after nurses he worked with noticed he was struggling to function. He was petrified. “He said: ‘I can't ever go back to that hospital. They'll crucify me. They'll say 'you made mistakes', and I'll be struck off’,” recalls Amandip. “Because he was signed off sick, he felt that he couldn't be a doctor anymore. That was his identity as an adult human being forcibly stopped, outside of his control.”
Amandip and his mother went to visit him that weekend. Though he wasn’t supposed to be working, he was still messaging his colleagues to give them notes about tests patients needed and chasing up unresolved problems. At this point, he was barely speaking to his family. He couldn’t even hold their gaze. Amandip uses the term “burnout” a lot to describe his brother’s condition at that time; “this level of physical, intellectual and emotional exhaustion, where you basically detach yourself from reality and life,” as he puts it. The more he mentions burnout, the more I start to think of it literally: imagining the wafer-thin ash left behind once a fire has burnt out, a breath of air away from crumbling completely.
As they left that Sunday, Amandip turned back to his brother. “I said, ‘don’t think of doing anything stupid’,” he recalls. “And as I looked at him, he just turned away.” It would be the last time he saw Jagdip alive.
As his car pulled into the car park, Amandip was astounded. The family had invited fewer than 50 people to Jagdip’s funeral, but the place was packed. A blur of faces he didn’t know. In the end, over 200 people had come, unannounced, to mourn Jagdip’s passing. The service was rammed, the crowd spilling out of the building. The vast majority of the mourners were people his brother worked with. In the blur of faces and condolences, he remembers a nurse coming up to him, saying “You'll never realise how much your brother was loved by us”.
The next day, a young-faced reporter knocked on Amandip's front door. He was one of two staffers from the Daily Mirror (the other had gone to Jagdip’s home); they wanted a comment on how his family were feeling about the death. ‘Death knocking’, as the controversial practice is known, is usually reserved for celebrities or major news figures. Amandip realised there was something else going on with the circumstances behind his brother’s death.
It was only in the weeks and months after the funeral that he came to learn fully of the conditions his brother had been working under. Running an entire cardiology department largely by himself, he would far exceed the hours outlined in his job description just trying to keep things going. Investigations into Jagdip’s death paint a picture of a hospital increasingly in disarray. He had no line manager to consult about the issues he was facing leading the department, as the role had been left unfilled at the trust, and he had been in a long running dispute with trust leadership over his training regime for new junior doctors. Meanwhile, that year Jagdip had to take over the patient lists of a fellow cardiologist who had left on long-term sick leave and the matron who worked closely with him to oversee the department was retiring — on the same day he was eventually signed off work. Major transformation programmes he had helped lead at the department had faced funding shortfalls after their grants were cut. He told colleagues he felt the department couldn’t cope with all the instability.
A recurring source of anxiety was the hospital’s performance targets. Jagdip feared the entire trust was set to be put into special measures as a result of its failures, and the weight of its targets was slowly weighing down on him. Colleagues reported after his death how they felt permanently under pressure from the NHS’ obsession with KPIs, with little leeway or understanding from management of the difficulty of achieving them with their stretched resources. Others reported feeling like a “resource being sweated” and suggested doctors had been turned into “factory workers” in an effort to deliver ever-increasing productivity. Not that there was much space to do this: doctors at the hospital had recently been pushed out of their old office space to make room for more beds.
After Jagdip’s death, the family met with the NHS trust that ran the hospital he had worked at. As he left the meeting, Amandip claims the trust’s chief executive asked him, almost nonchalantly, “Are you going to take legal action against us or not?” The trust’s internal investigation into the death acknowledged he had an “excessive workload” and was struggling with “the general demands of working within the resource-constrained NHS”. Jagdip was constantly worried about “access targets, delayed discharges and the financial situation of the trust”, it noted, and took these systemic problems as signs of a "personal failure”.
But instead of fully acknowledging that pressure, the report blamed Jagdip’s own inherent “isolation and inversion”, along with his failure to seek help to deal with them. The frustration he and other doctors felt towards targets were framed as signs of a “poverty of understanding” about real leadership. “The whole narrative was: 'we’re going to place the blame at his door. He was the one that chose to overwork. He overbooked his clinics. If he needed help, he should have put his hand up',” Amandip says. Jagdip was in an impossible situation, one that doctors and nurses up and down this country face every day: a hospital management obsessed with government-mandated performance and efficiency targets, coupled with a never-ending list of patients who needed his help, in an understaffed, underfunded and overburdened healthcare system.
In many ways, Jagdip could never escape his job. Amandip tells me, with frustration, how two strangers approached Jagdip when the brothers were at a wedding and started to recite a list of symptoms. Amandip wanted Jagdip to ignore them — he wasn’t at work after all, and he had to draw a line somewhere — but he didn’t. “That was his problem,” he says. “He would never say no.” Our ailing healthcare system relies on these people — people who cannot refuse to help those in need. And in Jagdip, they found someone to plug the gaps left by chronic staff shortages, overdemand and slashed budgets. Until one day he had nothing left to give.
Medical workers have been found to be disproportionately at risk of suicide. An NHS doctor dies by suicide every three weeks. A nurse attempts suicide almost every day. Even during the height of the pandemic, as the virus ravaged frontline healthcare workers, government data revealed that NHS staff took more sick days for mental health reasons than for Covid.
While there is no definitive evidence of what’s causing this phenomenon, there’s an increasing recognition that NHS working conditions could be a big part of it. In the decade after 2010, successive Conservative-led governments oversaw the largest sustained fall in NHS spending as a share of GDP since 1951. Today, the UK has fewer doctors, nurses and medical equipment per head than most comparable economies and half as many hospital beds as it had in 1987–88. Meanwhile demand has only gone up: the number of emergency-care admissions is more than twice the rate it was in 2010, and there is a backlog of 7.5 million people awaiting medical treatment.
Working somewhere that is permanently in disaster mode, where you spend all your time putting out fires, would take a lot out of anyone. But the altruistic nature of the medical profession only makes it worse. Healthcare workers often report feeling personally responsible for the systemic failures that mean they have to provide rushed or substandard care. It weighs on the mind. There’s a term for it now: moral injury. This can be compounded by the taboo around mental health among medical workers, in part driven by a sense of invulnerability; that those with a responsibility to keep others healthy can’t succumb to the conditions they diagnose in others. And it can be difficult to seek help when working in a hospital or NHS trust that doesn’t seem to support staff; places where medics can feel like they can’t speak up about problems without facing ramifications. These might be professional — the risk of losing the job that has become such a central part of their identity — or personal, in the guilt that can result from being unable to deliver adequate care.
In the years since the death of Jagdip, his brother has been left with a long list of unanswered questions. One that sticks with him, though, is: why Beachy Head?
The cliffside spot has become one of the UK’s best-known suicide spots. But why did Jagdip — who lived a two-hour drive away — feel the need to travel so far from home to end his life. One part of it, Amandip thinks, was likely that he didn’t want his body to be taken back to the hospital where he worked, so as not to add another burden to the people he worked with. But he can’t escape the idea that his brother was trying to send a message by choosing such a well-known and public place. “Look what happened to me. Don’t let this happen to you,” he says. “I know him, I know that’s exactly what he would be trying to say.”
“I thought, well, if he's no longer here to send that message, then it's my duty to send it for him,” Amandip tells me, with a look of grim determination. He took a year off work back in 2019 and ploughed his life savings to launch a new project, Doctors In Distress, a charity aimed at raising the alarm about the scale of suicides among medical staff and strategising about how to stem the tide.
It started with Amandip touring crowded rooms of NHS staff, sharing his brother’s story. Now Doctors in Distress runs frontline support sessions for doctors and nurses and advises on policy. Among the charity’s patrons is former doctor Adam Kay, who wrote the Bafta-winning TV show This Is Going to Hurt, a semi-fictionalised drama about Kay’s own experiences in the NHS (and, coincidentally, filmed at the Ealing Hospital where Jagdip once worked), in which one of the two protagonists dies by suicide. In the final episode, Kay’s character, played by Ben Whishaw, gives an impassioned speech about his friend’s death to a room of health service bureaucrats. “The idea of carrying on working in a broken system under shoddy conditions didn’t feel like any kind of future [to her],” he tells them. “One doctor takes their own life every three weeks. It should be a national fucking headline every time it happens, but instead it gets brushed under the carpet.”

The show premiered in 2022, at a time of unprecedented levels of pandemic-driven support for the wellbeing of medical staff. “The sad thing is, that's completely evaporated,” says Amandip. He highlights the Labour government’s health system reforms, centred around delivering more efficiency and productivity from doctors; “so patients get more out of it for what taxpayers put in,” as Health Secretary Wes Streeting recently put it. But what will that mean for overburdened doctors and nurses? What is efficiency if not asking people to do more with less?
Amid Covid amnesia, productivity drives and frustration at long waiting times, we’ve moved back, publicly and politically, to a technical discussion about the NHS that focuses solely on input and output; the money we put in and the performance for patients. In doing so, we forget the human components that keep its wheels turning, even as the conditions they work under are more overwhelming than ever. In the meantime, more and more doctors share Jagdip’s fate.
Six years on from his death, Amandip still gets messages from his brother’s former patients, telling him what a good doctor his brother was. The most recent one reached out on LinkedIn just a couple of months ago. “His patients are still here and alive today. That was all down to him,” Amandip says. “That’s his biggest legacy.”
In the UK, Samaritans can be contacted on freephone 116 123. Visit Samaritans.org for more information. Other international helplines can be found at befrienders.org. A list of LGBTQIA+ mental health helplines can be found at Mind.

Comments
How to comment:
If you are already a member,
click here to sign in
and leave a comment.
If you aren't a member,
sign up here
to be able to leave a comment.
To add your photo, click here to create a profile on Gravatar.






